Stories
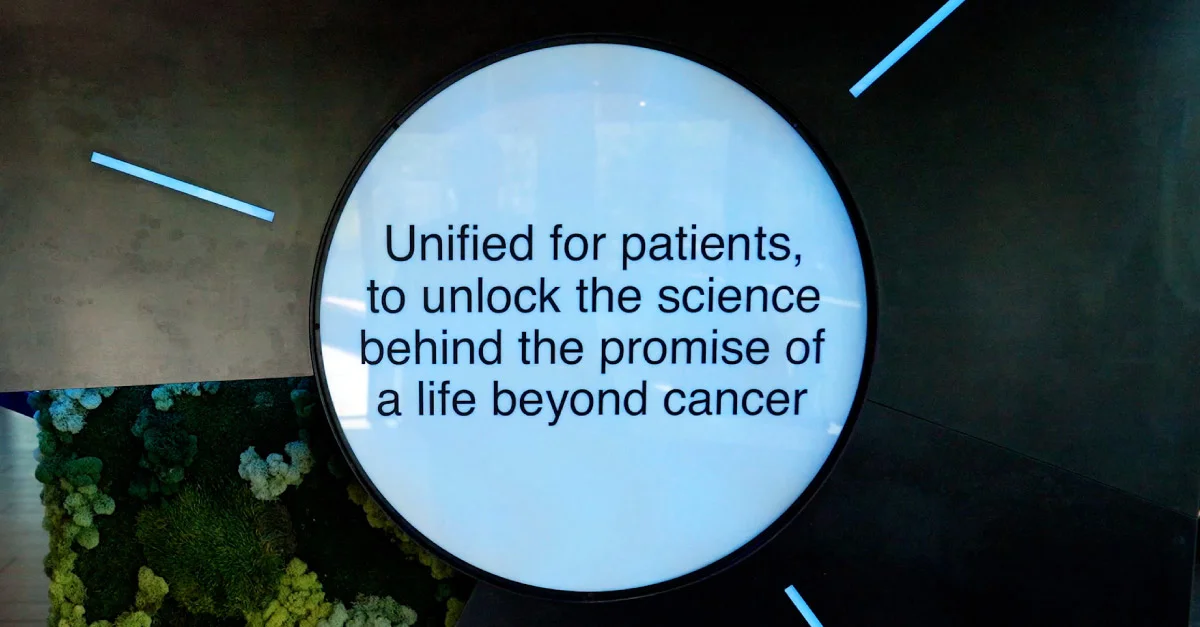
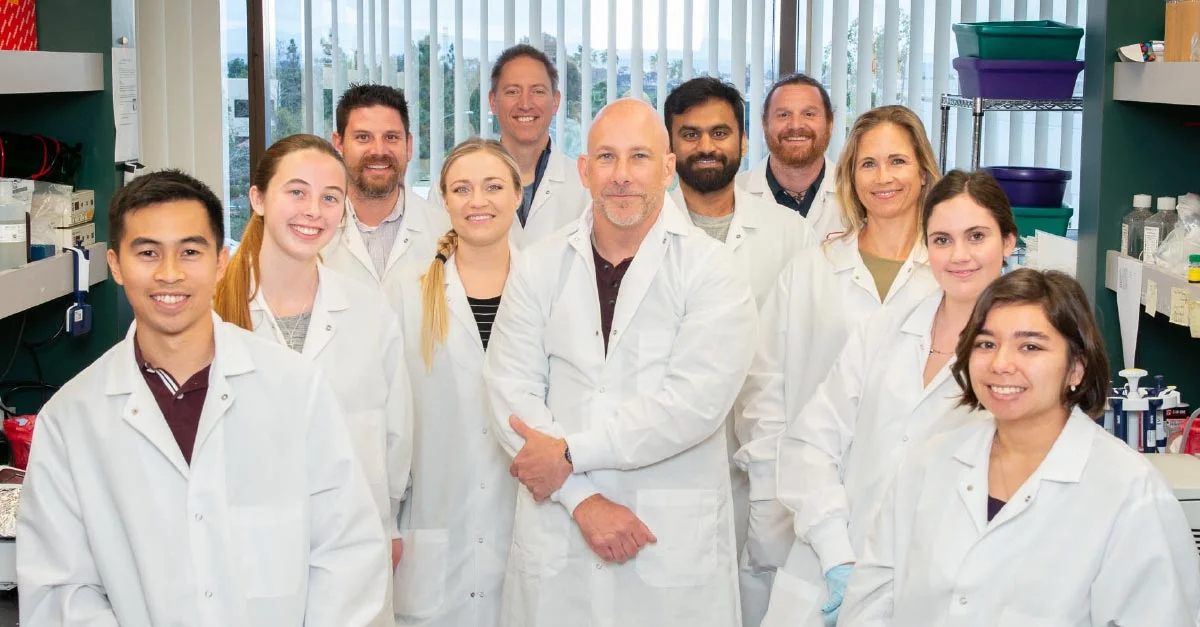
Beyond relevant information about Mirati’s path to innovation for patients, our humanizing journalism showcases the work of our employees.
Beyond relevant information about Mirati’s path to innovation for patients, our humanizing journalism showcases the work of our employees.
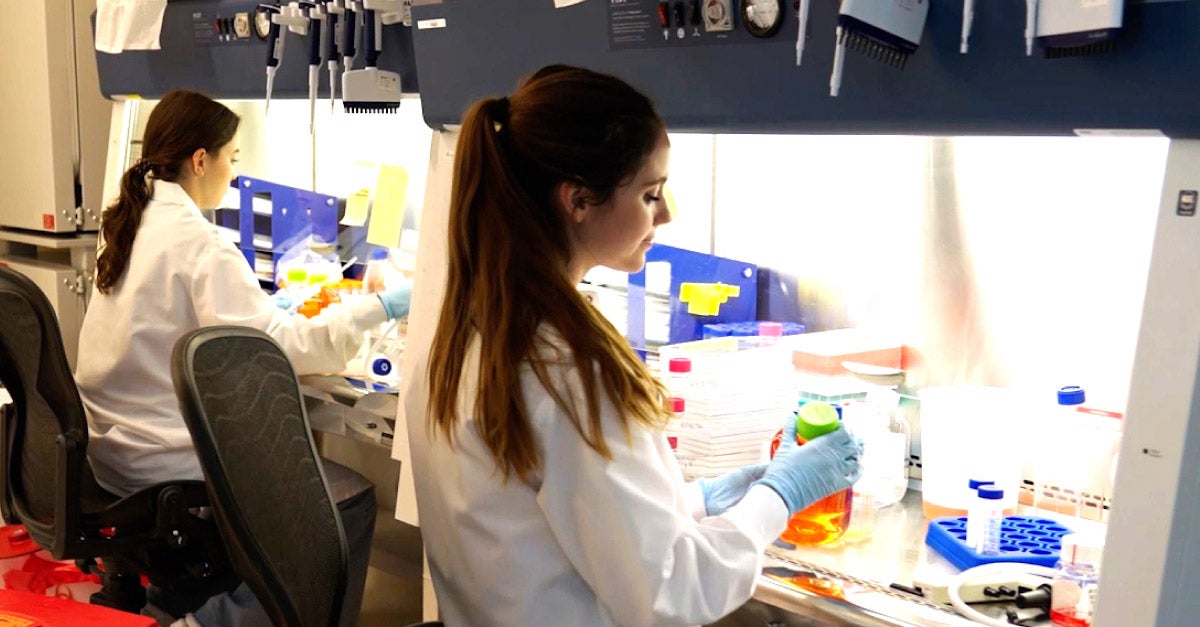
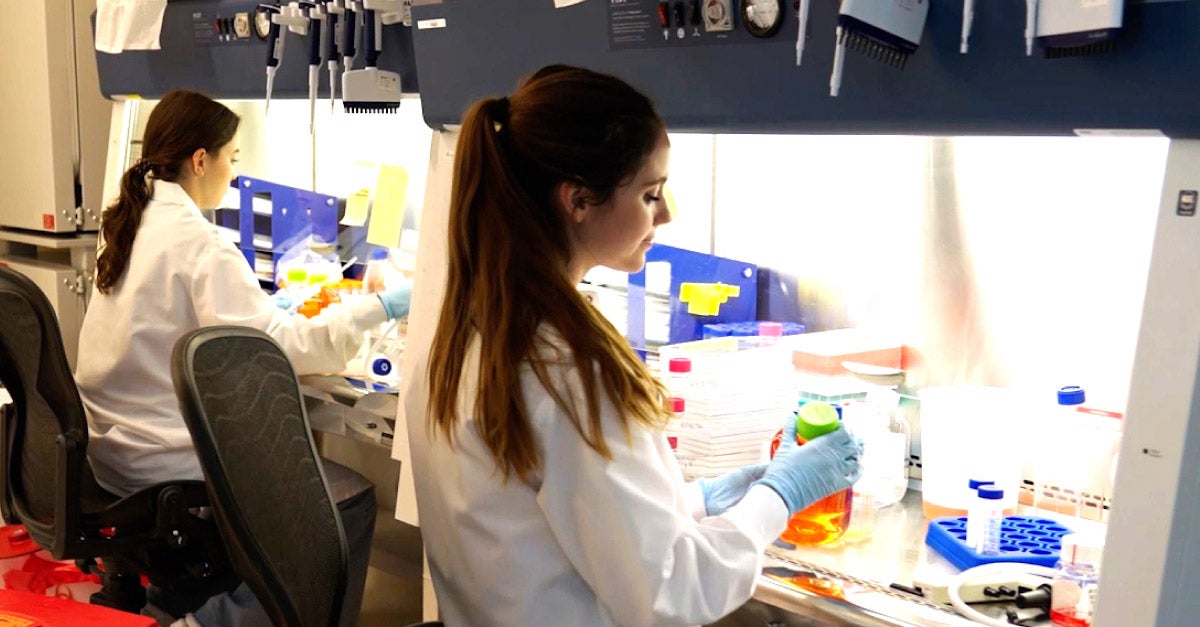
People & Culture
Learn more about how our team shows up.
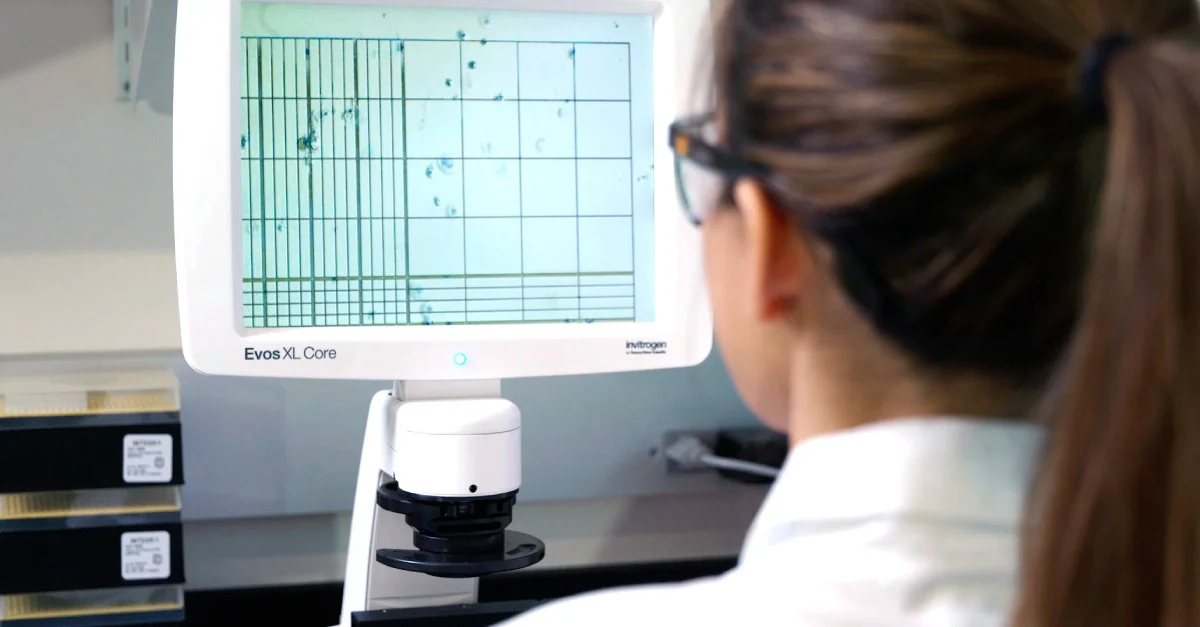
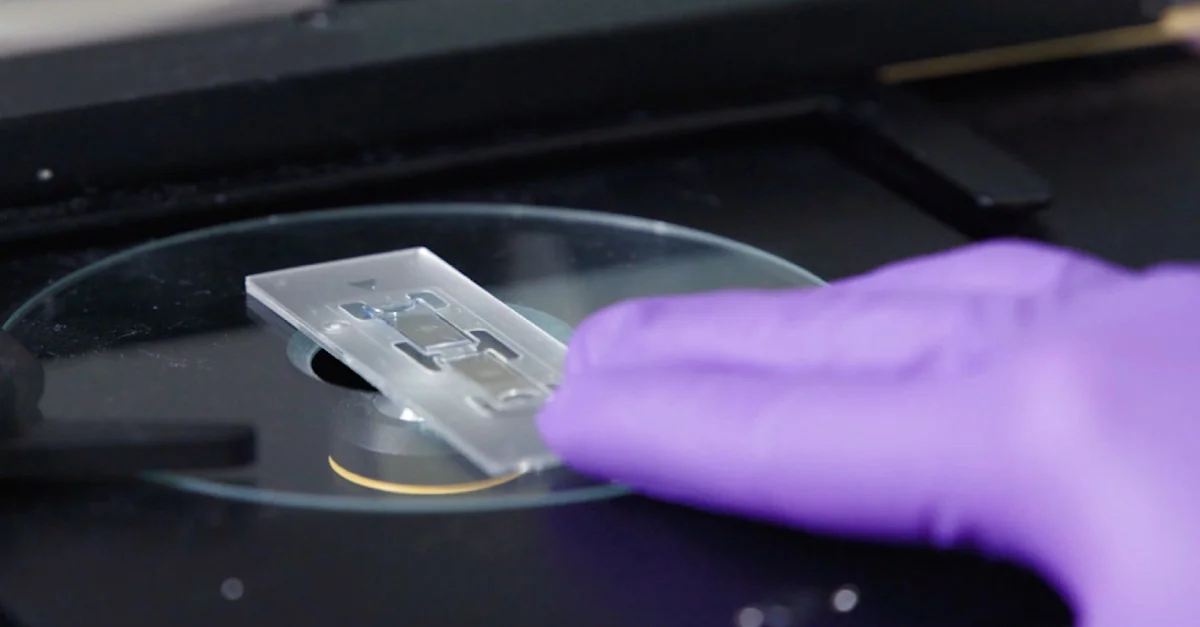
Science
Learn more about our science.
Citizenship
Read more about how our impact goes beyond discovering, developing, and delivering medicines.



Perspectives
Read about our take on trending topics that impact our work and patients.
People & Culture
Learn more about how our team shows up.








Science
Learn more about our science.





Citizenship
Read more about how our impact goes beyond discovering, developing, and delivering medicines.



Perspectives
Read about our take on trending topics that impact our work and patients.

















Topic: Advocacy





Topic: Careers







Topic: Collaboration



Topic: Culture









Topic: KRAS






Topic: R&D